Contrast extravasation after major trauma can be very problematic. Extravasation into a solid organ (liver, spleen) generally requires a quick trip to interventional radiology or the operating room. Bleeding from the bowel mesentery assures an exploratory laparotomy. Gluteal vessel extravasation is best treated with angioembolization.
But what about extravasation from off the beaten path areas like the psoas muscle? This is an uncommon finding on trauma CT, so less is known about the usual clinical course. A group in Okayama Japan performed a 10-year retrospective review of data from their hospital. They reviewed hematoma size, associated injuries, and the relationship to treatment options.
Here are the factoids:
- 762 contrast CTs were performed due to blunt trauma over the 10 year period (only 76 per year?!)
- About 15% (117 patients) had either lumbar process fracture or psoas hematoma, and about one quarter had obvious contrast extravasation into the muscle
- Patients with contrast extravasation were significantly older, had higher ISS, and were more likely to require transfusion
- There was an association between the number of transverse process fractures and “need for” angioembolization
- Size of the psoas hematoma was predictive of the need for angioembolization
- Angioembolization of the psoas was frequently associated with embolization of the pelvis
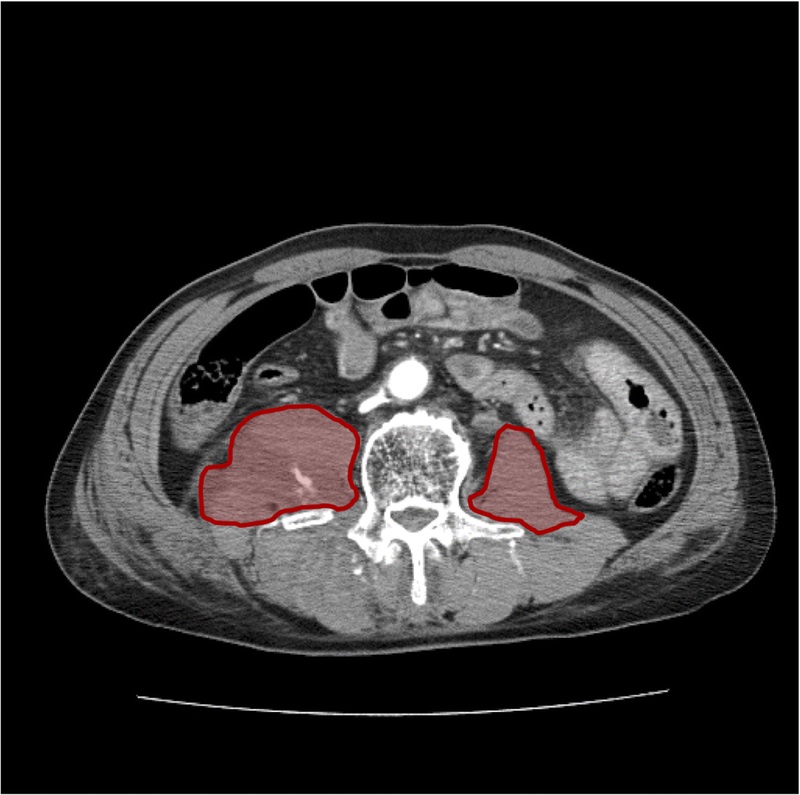
The right psoas has both contrast extravasation and a sizable hematoma
Bottom line: This study has many weaknesses, but does show that psoas extravasation occurs somewhat frequently, even at a low volume center. I always worry about studies that state something like “and xx patients required intervention.” Generally, this means that it was performed at the discretion of the clinician and no consistent rules were applied. And even though hematoma size was significantly correlated with angioembolization, it’s probably not worth the effort to have your radiologist calculate it. But it does illustrate one nearly universal trauma rule:
Patients with active extravasation on CT are bleeding to death until proven otherwise
Do not sit back and manage expectantly! The corollary to this rule is:
Contrast extravasation on CT always requires active measures to stop it
These active measures are typically angioembolization for difficult to reach areas in hemodynamically stable patients (gluteal artery for buttock, lumbar artery for psoas muscle, solid organs). Unstable patients absolutely require a trip to the OR for control. Superficial muscular bleeding frequently stops with good pressure dressings or positioning the patient so they lie on the affected area. Just don’t sit around and watch these patients bleed when you see extravasation on the CT.
Reference: Impact of contrast extravasation on computed tomography of thepsoas major muscle in patients with blunt torso trauma. J Trauma 86(2):268-273, 2019.
