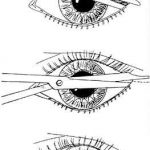
Lateral Canthotomy For Orbital Compartment Syndrome
I’ve previously written about the orbital compartment syndrome and described the symptoms in the awake patient. I’d like to share a video of the procedure and provide a tip for diagnosing it in unconscious patients.
Patients at risk will have obvious facial trauma. During your physical exam, look for proptosis. This is caused by swelling or hemorrhage behind the globe pushing it forward. It may manifest itself as uneven opening of the eyelids, with the affected side being “propped” open (get it?). But in trauma, there may be significant edema which keeps the lid closed.
The easiest way to observe proptosis is to stand above the patients head, looking toward their feet. Crouch down so you can look across the lids in a direction horizontal to the floor. You should easily be able to detect if one eye protrudes further that the other.
You can also do a poor man’s compartment pressure test by gently using your thumbs to compress both globes simultaneously. If there is substantial difference in resistance between the two sides, a compartment syndrome may be present. Important note! Do a thorough globe exam first! If there is any evidence of globe rupture (hyphema, irregular pupil, extra tissue in the anterior compartment), don’t press the eye or perform a canthotomy. CT scan of the facial bones can help confirm the diagnosis if a mass effect is seen in the orbit or if the optic nerve appears to be on stretch.
The orbital compartment syndrome is an emergency! Once diagnosed, immediately proceed to canthotomy. Otherwise, damage to the optic nerve and retina is likely, and the patient may become blind in the affected eye.
Related post: