Tissue oxygenation is critical to wound healing. But unfortunately, there is no easy way to “see” how healthy the wound is just by looking at it. A research team at the Massachusetts General Hospital is developing a spray-on “smart” bandage that determine, at a glance, shows a map of tissue oxygen levels.
Now, of course, the researchers had to get clever and come up with a lame acronym. So here it is: sensing, monitoring and release of therapeutics (SMART). Get it? SMART bandage.
Here’s what it looks like:
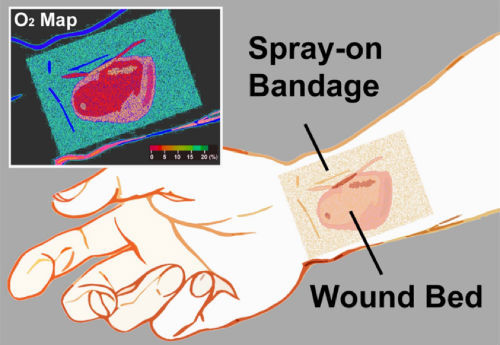
Okay, so how does it work? There are three components: a sensor molecule that glows over a useful range of oxygenation values, a bandage material to bind it to, and an imaging device for capturing useful images.
The sensor molecule is a phospor derivative that glows longer and brighter as tissue oxygen decreases. The bandage is a viscous liquid that is painted on the skin and dries as a solid film within a minute (think NewSkin). It contains the sensor molecule. In order to keep room air from seeping into the bandage and interfering with the readings, a transparent barrier is placed over it (think Tegaderm).
Finally, the detector is … a smartphone or camera! No need for other expensive equipment. The flash stimulates the phosphors as the image is recorded. The image can then be analyzed for brightness and color of the phosphors.
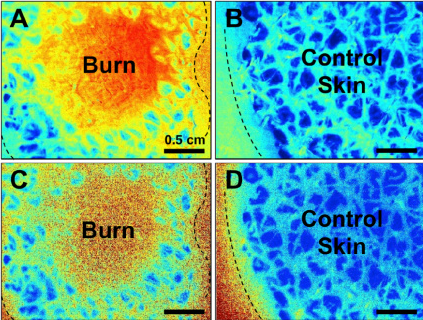
What is this good for? Trauma professionals deal with soft tissue wounds on a regular basis. Some of the more complicated ones require skin grafts or flaps, and maintaining their health is very important. Imagine begin able to identify oxygenation problems early in the edges of a flap or from a small seroma under a skin graft. This could lead to earlier correction of any problems and an increase in graft salvage. And it may allow us to better predict which burns are getting worse or may need grafting. Here are images of burn vs normal skin:
Bottom line: Yet another cool (and probably inexpensive) tool in expanding our senses to appreciate factors that help wound healing. Once the kinks are worked out, expect this to move into clinical care fairly quickly.
Related posts:
Reference: Non-invasive transdermal two-dimensional mapping of cutaneous oxygenation with a rapid-drying liquid bandage. Biomedical Optics Express 5(11):3748-3764, 2014.

