Governmental agencies everywhere collect trauma related data. The US federal government maintains a number of databases, such as the Fatal Accident Reporting System (FARS), the Census of Fatal Occupational Injuries (CFOI) and many others. States collect similar but smaller datasets. Even towns and municipalities collate injury information in the form of prehospital run sheets.
But reams of data are of no use unless you can learn something from it. Unfortunately, most of this data is tucked away in database management systems, or in some cases just stacks of paper forms locked up somewhere. In order for humans to make sense of it and do useful things with it, we need to transform it into forms that we can easily interpret and make sense of.
Fortunately, there are lots of visual, electronic tools available to help us do just that. One of the most helpful tools is the programmable geographic information system (GIS). An example of this is Google Maps. Most of us have used this or a similar tool in some form, usually to get directions from here to there. But you may not be aware that Google provides a programming interface so a savvy user can place any type of geography-related data on the map, creating what is called a mashup.
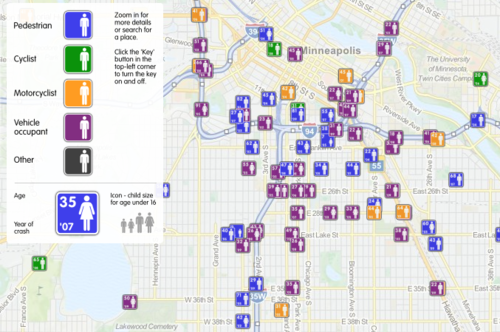
Imagine crossing the FARS database, which contains extensive data points on every fatal road accident in the US, with a mapping system. This would allow creation of a map showing where every person lost their life in a road accident, along with additional pertinent information about the event. A great example of this is demonstrated below. It was created by ITO World Ltd., based in the UK. They crossed fatality information with geographic map data in both the US and the UK.
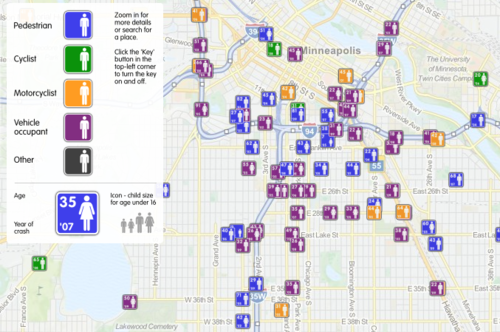
This map shows fatal road events around Minneapolis from 2001 to 2009. The type of event (pedestrian struck, motor vehicle crash, etc.) is displayed along with age, year and sex. It is movable and zoomable so it can be viewed it in great detail. Click on the map above to open a new window to the full map.
Bottom line: Using trauma data / map mashups is a great way to visualize complex information. It also allows us to plan meaningful prevention activities based on local information (a requirement for ACS trauma center verification). Imagine looking over such a map of your city, and identifying a cluster of pedestrian fatalities. Then you notice that this cluster is 2 blocks away from an elementary school. This could prompt you to work with the school to implement automobile awareness programs for the children, have the city review signage and obstructions to view in the area, and optimize the number and placement of crossing guards. Then redo the map afterwards to judge the impact. Wow!
Website: http://map.itoworld.com/road-casualties-usa#fullscreen
Reference: Using geographic information systems in injury research. J Nurs Scholarsh 39(4):306-311, 2007.