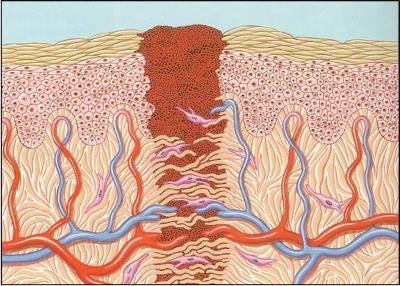
At some point in their training, every trauma professional is taught that there is a certain period time during which a wound can be safely closed. The exact number varies, but is usually somewhere between 6 and 24 hours. After that, we are told, “bad things happen.”
Always question dogma, I say. Is this true, or is it another one of those “facts” that have been propagated through the ages? Two emergency medicine groups recently performed a meta-analysis to try to answer my question. As usual, they found that much of the published literature is not very good. Out of 418 papers in their original search, only 4 fully met their criteria (laceration repaired primarily, in the ED, with clear early vs delayed criteria.
With the exception of one study with a very limited focus, there was no correlation between wound age and infection or dehiscence after primary closure. None of the studies could reliably provide a specific time beyond which closure was destined to fail. And the use of antibiotics in some of the studies also confounded the results.
Bottom line: It is more likely that infection-prone wounds get infected, not old ones. Although leaving a wound open to heal by secondary intention usually avoids the problem, it’s a big patient dissatisfier, especially with large wounds. Since many patients don’t present to the ED until their wound is “old”, it may be reasonable to try primary closure in all but infection-prone wounds. (The meaning of that phrase is not exactly clear, but most of us know it when we see it.)
Reference: The impact of wound age on the infection rate of simple lacerations repaired in the emergency department. Injury 43(11):1793-1798, 2012.