In the previous post, I reviewed some basic information on DOAC reversal. Five years ago, it was costly and questionably effective. So what has happened in the meantime?
In this post, I’ll review a big trial the pharma company was excited about and make a few comments.
ANNEXA-I Study
This study sought to evaluate the hemostatic effect of Andexanet administration in patients taking a Factor Xa inhibitor who suffered an intracranial hemorrhage.
Key points in this study:
- It was a five-year, multicenter, randomized controlled trial
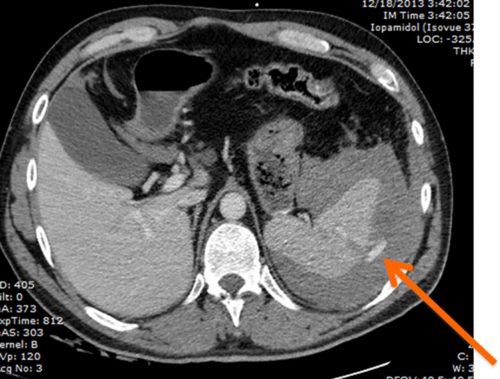
- Subjects had to have taken their medication within 15 hours of the event, had an intracranial hemorrhage identified by CT within 12 hours of symptoms, and randomized in the study within two hours after the scan
- There were 263 patients reversed with Andexanet and 267 with “usual care,” which was not clearly defined aside from administration of prothrombin complex concentrate (PCC)
- Traumatic ICH was only present in about 13% of subjects, and the average volume was about 10 mL. Most were intracerebral hemorrhages (90%), with 5% or less being subdural hematomas.
- Andexanet treatment was associated with increased “hemostatic efficacy,” a combination variable consisting of volume change, change in NIH Stroke Scale score, and no need for rescue therapy within 12 hours. There was also decreased hematoma volume change by 3.8mm (12%), an increased number of thrombotic events (10% vs. 6%), and an increased number of ischemic strokes (6.5% vs. 1.5%) at 30 days. There was no difference in deaths at 30 days.
- Hemostatic efficacy was highest in intracerebral hemorrhages and nearly ineffective for subdural hematomas
- Hemostatic efficacy was significantly higher than that of patients who received PCC in the “usual care” arm, but it was no better than usual care without PCC (?)
Bottom line: Wow! That’s a lot of numbers. The company was excited because the trial was stopped early due to “superior [hemostatic] efficacy vs usual care.” Basically, what they are saying is that the combination of hematoma size, stroke scale, and lack of need for other rescue therapy was significantly lower in patients treated with andexanet alfa.
But is this meaningful in trauma? There are several issues, IMHO:
- The study was not powered to detect mortality or functional outcome differences, which is what we trauma people are really interested in
- The primary outcome (hemostatic efficacy) was powered mainly by hematoma size change, which is not of any clear clinical significance
- There were some shenanigans from company involvement in the study design, with several protocol amendments that occurred
- It was not clear what “usual care” consisted of other than PCC administration in some patients
- There was no information on costs
In my next post, I’ll cite several systemic reviews and meta-analyses to come to some final conclusions about this drug.
Reference: Andexanet for factor xa Inhibitor–Associated acute intracerebral hemorrhage. N Engl J Med. 2024;390(19):1745-1755.