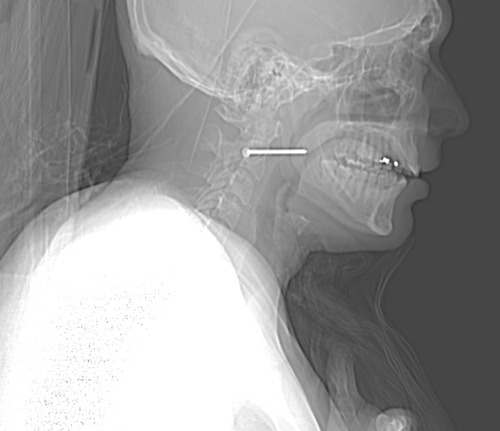
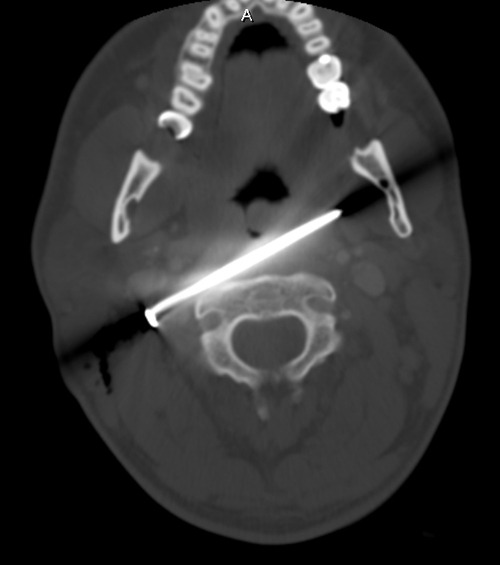
We’ve made sure that our victim of the nail gun to the neck did not need an emergent operation. Vitals are stable, there’s no uncontrolled hemorrhage, and the patient is neurologically intact. We’ve imaged him using CT angiography, and the nail does not appear to have injured any vital structures.
How do we get it out of there? There are two things that need to be considered: where and how.
Rule of thumb: If a foreign body is located anywhere near vital structures, take it out in the OR, no matter how good you think the imaging is. It may be tempting to just pull it out in the ED, but resist! CT scans look so good, and they are so detailed, but they are not perfect. The ED does not have the equipment, personnel, or lighting necessary if something goes awry.
Rule of thumb: Use all information available to plan the removal procedure. In this case, the head of the nail is to the patient’s right. Therefore, it must be removed from the right side. The CT shows that the nail passes very close to the posterior pharynx, so it will need to be evaluated during the procedure.
This patient was taken to the operating room. During the intubation, direct laryngoscopy was carried out to carefully inspect the entire pharynx and larynx. No evidence of penetration was seen. The entire neck, face, and upper chest were prepped and draped (I like to go overboard in trauma cases; you never know what is going to happen). Fluoroscopy was available.
The classic operation would have been to make an incision along the sternocleidomastoid on the right side. The nail head would be approached directly. Since long, thin objects can be notoriously difficult to locate, fluoro can be very helpful. The exact position with respect to the carotid and jugular can be ascertained. Then the nail head is grasped with a clamp, and the nail gently pulled out along its axis. A nice, long wait for any evidence of bleeding should occur. The area can then be irrigated and the incision closed. Skin antibiotics can be given postop, but only one dose at most.
Having said that, I opted for a different approach based on an old blog post here. Tune in on Wednesday to see what I really did.