Yesterday, I wrote about the accepted management of and delay in flying due to traumatic pneumothorax. I republished the post because of the very recent acceptance for publication of a paper from Oregon Health Science University in Portland. The authors specifically tried to assess timing of chest tube removal and long-distance flight, and to measure the risk of pneumothorax recurrence or other complications.
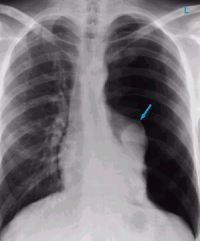
The authors performed a retrospective review of a series of military patients who had sustained chest injuries that were treated with chest tubes over a 5 year period from 2008 to 2012. After tube removal and a pneumothorax-free period of at least 24 hours (by chest x-ray), the patients were then transported by air from the military theater back to the United States.
Here are the factoids:
- Of 517 patients screened in the military trauma registry database, only 73 were available for study after applying exclusion criteria
- Subjects were predominantly young and male, as one would expect from the injured military population, and 74% were injured by a penetrating mechanism
- Median time that the chest tube was in place was 4 days, and median time from tube removal to flight was 2.5 days
- All patients had post-flight documentation available for review, but only half (37) had in-flight documentation available
- Nearly half (40%) had positive pressure ventilation in place during the flight
- Five patients had “in-flight medical concerns” (4 were ventilated), but none were related to the pneumothorax. The four ventilated patients had ventilator issues, the non-vented patient had “self-limited discomfort without evidence of respiratory distress.”
- None of the subjects developed a recurrent pneumothorax, either post-flight or over the following 30 days
The authors conclude that air travel after tube removal and a 24-72 hour observation period “appears safe.”
Bottom line: Not so fast! This is yet another small, retrospective study making grand claims. The study group is a very unique population: healthy, fit young men with penetrating injury. Your average civilian trauma patient is older, less healthy, and usually has a blunt mechanism with multiple rib fractures. In-flight documentation was not available in half of the cases. And a full medical team was present on the aircraft had a problem actually occurred.
Contrast this with a civilian patient on a commercial aircraft with very limited medical equipment and expertise on board. What could go wrong? I definitely do not recommend changing our practice on these patients yet based on this one paper. Until we have better guidance (more good papers) stick to the usual wait time to ensure a safe flight for your patient.
Reference: Trauma patients are safe to fly 72 hours after tube thoracostomy removal. J Trauma, published ahead of print, May 18 2018.