I recently wrote about this journal article from a couple of pediatric trauma programs in New York. The article tried to focus on reducing the rate of phlebotomy in children who are being observed for solid organ injury. I was more excited about the overall protocol being used to manage liver and spleen injury, as it was a great advance over the original APSA guideline. But let’s look at the phlebotomy part as well.
This is an interestingly weird study, and you’ll see what I mean shortly. Two New York trauma hospitals that take care of pediatric patients pooled 4 years of registry records on children with isolated blunt liver and/or spleen injuries. Then they did a tabletop excercise, looking at “what if” they had applied the APSA guideline, and “what if” they had applied their new, proposed guideline.
Interestingly, this implies that they were using neither! I presume they are trying to justify (and push all their partners) to move to the new protocol from (probably) random, individual choice.
Here are the factoids:
- 120 records were identified across the 2 hospitals that met criteria
- Late presentation to the hospital, contrast extravasation, comorbidities, lack of imaging, operative intervention at an outside hospital excluded 59 patients, leaving 61 for analysis. Three of those patients became unstable and were also excluded.
- None of the remaining patients required operation or angioembolization
- Use of the “new” (proposed) protocol would reduce ICU admissions by 65%, reduce blood draws by 70%, and reduce hospital stay by 37%
- Conclusion: use of the protocol would eliminate the need for serial phlebotomy (huh?)
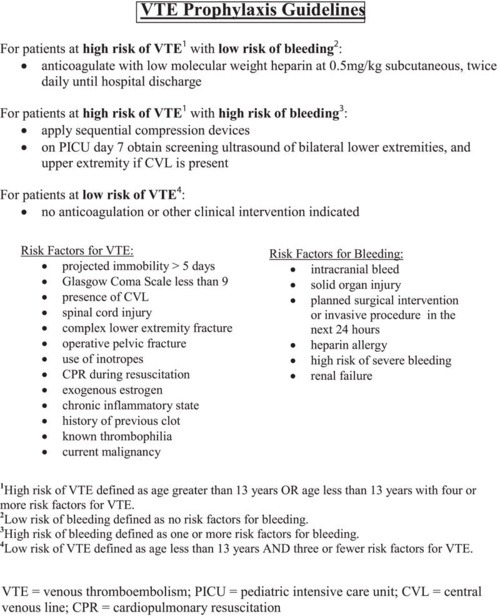
Bottom line: Huh? All this to justify decreasing blood draws? I know, kids hate needles, but the data on decreased length of stay in the hospital and ICU is much more important! We’ve been using a protocol similar to their “new” one at Regions Hospital, which I’ve shared below. We’ve been enjoying decreased resource utilization, blood draws, and very short lengths of stay for over a decade. And our analysis showed that we save $1000 for every patient entering the protocol, compared to the old-fashioned and inefficient way we used to manage them.
Related posts:
- Phlebotomy and pediatric solid organ injury – Part 1
- Printable version of the New York protocol
- Regions Hospital solid organ management protocol – adult
- Regions Hospital solid organ management protocol – peds
Reference: Reducing scheduled phlebotomy in stable pediatric patients with liver or spleen injury. J Ped Surg 49(5):759-762, 2014.