Treating Pneumothorax With Oxygen (Again)
The topic of treating pneumothorax with high inspired oxygen concentrations keeps coming up! I’ve written about this a few times in the past, and the literature I found supporting the practice was terrible. Some readers brought three more studies to my attention that support it, so I’m going to take the next three days to see if there is any hope for this practice.
Today’s paper used a rabbit model where each animal was given a complete pneumothorax by the injection of 15cc (!!) of air into one hemithorax. The authors then let the pneumothorax resolve using room air or 30%, 40%, or 50% FIO2. Each group consisted of 10 rabbits, and repeat chest xrays were obtained every 6-8 hours to follow resolution.
The statistical analysis was interesting and unusual. Because the authors were studying the time to resolved pneumothorax with higher inspired O2, they were looking for a test that would analyze an “ordered alternative.” The Jonckheere-Terpstra test was used, which I have never heard of, but I’ll assume it’s the legitimate one to use.
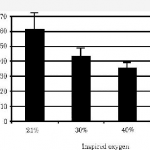
The figure at the top of this post shows the results. Looks promising right? There was a big improvement from room air to 30%, but lesser improvement using higher oxygen concentrations. The error bars (standard error of the mean) are remarkably tight, but this makes sense since xrays were only being taken every 6-8 hours.
The two big problems with this study are that: 1. they’re rabbits and it only takes 15cc of air to drop the entire lung, and 2. standard xray is being used to measure resolution. Trying to pick apart the exact time to resolution of a 15cc pneumothorax is very difficult, and to try to do it with a test that we know is not great at detecting small amounts of air even in big humans just doesn’t work.
Bottom line: Fancy statistics and nice looking results don’t make up for an animal model that doesn’t necessarily correlate with humans and deriving results using an inaccurate diagnostic test. Tomorrow, I’ll look at a paper in the Journal of Pediatric Surgery to see if it fares any better.
Related posts:
Reference: Resolution of experimental pneumothorax in rabbits by graded oxygen therapy. J Trauma 45(2):333-334, 1998.
Thanks to Stephanie Taft MD at Regions Hospital for finding these fine studies for me.