Syncope accounts for 1-2% of all ED visits, and is a factor in some patients with blunt trauma, especially the elderly. If syncope is suspected, a “syncope workup” is frequently ordered. Just what this consists of is poorly defined. Even less understood is how useful the syncope workup really is.
Researchers at Yale retrospectively looked at their experience doing syncope workups in trauma patients. They were interested in seeing what was typically ordered, if it was clinically useful, and if it impacted length of stay.
A total of 14% of trauma patients had syncope as a possible contributor to their injury. The investigators found that the following tests were typically ordered in these patients:
- Carotid ultrasound (96%)
- 2D Echo (96%)
- Cardiac enzymes (81%)
- Cardiology consult (23%)
- Neurology consult (11%)
- EEG (7%)
- MRI (6%)
Most of this testing was normal. About 3% of cardiac enzymes were abnormal, as were 5% of carotid imaging and 4% of echocardiograms.
Important! Of the patients who underwent an intervention after workup, 69% could have been identified based on history, physical exam, or EKG and did not depend on any of the other diagnostic tests.
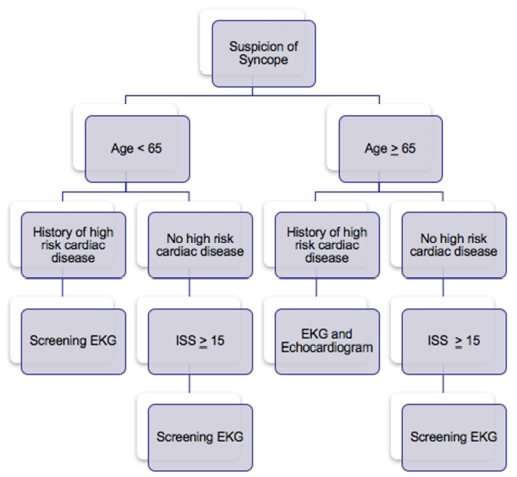
Is it possible to determine a subset of this population that may show a higher yield for this screening? Surgeons at Temple University in Philadelphia found that there was little utility in using carotid duplex studies. They did note that patients with a history of heart disease were more likely to have an abnormal EKG, and that an abnormal EKG predicted an abnormal echo. Overall, only patients with a history of significant cardiac comorbidity, older age, and higher ISS had findings requiring intervention.
Bottom line: Don’t just reflexively order a syncope workup when there is a question of this problem. Think about it first, because the majority of these studies are nonproductive. They are not needed routinely in trauma patients with “syncope” as a contributing factor. Obtain a good cardiac history, and if indicated, order an EKG and go from there. See the practice guideline proposed by the Temple group below. And be sure to include the patients primary doctor in the loop!
References:
- Routine or protocol evaluation of trauma patients with suspected syncope is unnecessary. J Trauma 70(2):428-432, 2011.
- Syncope workup: Greater yield in select trauma population. Intl J Surg, accepted for publication June 27, 2017.