Trauma performance improvement (PI) is a rigorous system that ensures high quality care of trauma patients. For the next three days I’ll be digging into the final goal of the process, loop closure. Today I’ll talk about what loop closure really is. And remember, this process applies to all phases of care from prehospital to post-discharge.
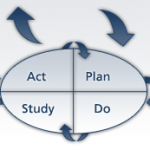
Your trauma PI program basically identifies problems of any type, requires someone to come up with potential solutions, applies these solutions, then monitors the result. This process is a cycle, since the first solution may only partially solve the problem. The initial solution may need to be tweaked or totally changed. This loop continues until a reasonable result has been achieved.
Loop closure is really two things: achievement of the best possible resolution of the initial problem, and documentation of the process. One is not possible without the other. A common trauma PI problem I encounter is documentation of “loop closure” when the original problem is still recurring.
When most people talk about loop closure, they are usually referring to the documentation part. Each PI problem must have a discrete “folder” of documentation that details every step of the process, from recognition to closure. This folder may reside securely on a computer (remember to back up regularly), or it can be a good old-fashioned manila folder.
The documents that are saved vary depending on the specific problem that was addressed. However, typical materials may include meeting minutes, registry reports, personnel letters, email messages, and protocols. I will give specific examples of the documents that should be included tomorrow and Wednesday.
All related documents should be included in the folder for that specific issue. All PI issue folders should then be kept in a single location, not spread across several binders or locations. Multiple people in your trauma program should be familiar with the PI folder organization. Otherwise, what happens if your Trauma Program Manager, who has been with you for years and is the only one that really understands how PI is organized, decides to retire or move to another trauma program? Your entire program may be in jeopardy.
Related posts:
- Loop closure (Part I)
- Peer-related loop closure (Part II)
- System issue loop closure (Part III)
- Peer issue vs system issue (Part IV)
Please email any specific questions you have, and I’ll answer those on Thursday and Friday.