Spinal cord injuries are typically devastating injuries with profound consequences for function and life expectancy. However, a small percentage result in rapidly reversible symptoms. Because these temporary injuries are rare, they tend to cause confusion among clinicians.
Technically, a spinal cord concussion (a “zinger” or “stinger” is an example) is a mild cord injury that results in transient neurologic disturbances. The deficits can be sensory, motor or both, and typically resolve in less than 48 hours. The injuries tend to involve the mid-portion of the cervical cord or the cervico-thoracic junction, since these are the areas of maximum mobility. In a few cases, the athlete has congenital narrowing of the spinal canal which predisposes them to injury. In most cases, the injury probably occurs due to the flexibility of the young spine.
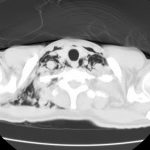
The usual management consists of an MRI of the spine followed by admission and frequent neurologic checks to ensure ongoing resolution. MRI is typically negative in a true concussion. If a signal change is seen, then technically a cord contusion is present. Management is the same for both. There is no indication to give steroids. Evaluation of the ligaments is critical to determine if a collar will be necessary.
Recovery is rapid and complete. But what is the answer to the inevitable question, “when can he/she return to play?” In adult players, the literature suggests that it may be safe to return once they have fully recovered. There is little guidance for kids.
Here’s what I tell the parents: This event has shown that, given the right force applied to your child’s neck, the bones can move enough to injure their spinal cord. This time, the cord was just tickled a little bit. But if the bones had moved just another millimeter or two, this injury could have been permanent and they would never have walked again. I recommend that they do not play this sport again.
Some of you may disagree. I’d be very interested in hearing your comments.
Reference:
- First mention: About concussion of the spinal cord. Wein Med Jahrb 34:531, 1879.