The patient impaled himself in the thigh while climbing over a wrought iron fence. A section of the fence (including him) has been carefully been separated, and it’s been secured while he is loaded into the ambulance. He’s just been dropped at your emergency department. What to do?
Trauma team activation? Yes! This should have been called in advance so the team could assemble prior to the patient’s arrival. This will definitely require a team, and the surgeon will be essential in planning further care.
Sedation? Definitely! If the embedded object is unwieldy or causes much discomfort, even consider electively sedating and intubating the patient for ease of management without causing more pain.
OR activation? Yes! Even before the patient arrives, the surgeon should call the OR to ready a room, since this will almost certainly require surgical attention.
ATLS guidelines? Yes! This case presents a perfect example of the Dang! factor (see below). Don’t let the team focus attention on the dramatic problem while ignoring his impending airway obstruction or some other major problem. A good physical exam of the involved part is essential to detect any subtle neurovascular symptoms that may give clues to deeper injuries.
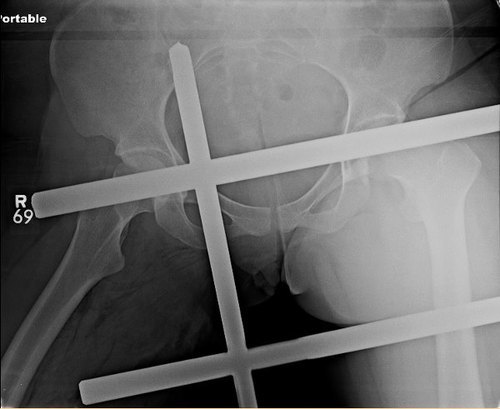
Imaging? Maybe. Only if it will provide information that would help guide the extraction process. Just remember, it’s iron. Most radiographs and any MRI will be significantly degraded by so much metal.

The top left bar was in the groin crease, the middle left bar pierced the back of the thigh. There were no vessels or nerves involved.
Extraction in OR? Almost always! Only the smallest object embedded in the most benign areas can be removed in any place other than the OR. Depending on how close the foreign body is to any vital structure, the surgeon needs to decide whether to cut down on the object vs sliding it out and watching for the consequences (bleeding). Tourniquets may be used in more distal areas (not this case, though, due to how proximal it is).
Related posts: