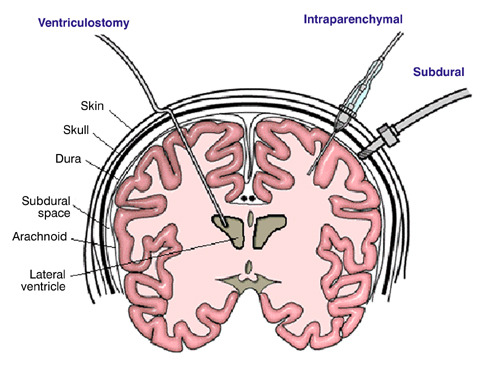
Management of severe traumatic brain injury (TBI) routinely involves monitoring and control of cerebral perfusion pressure. Monitoring is typically accomplished with an invasive monitor, with the extraventricular drain (EVD) and fiberoptic intraparenchymal monitors (IP) being the most common.
The extraventricular drain is preferred in many centers because it not only monitors pressures, but it can also be used to drain cerebrospinal fluid (CSF) to actively try to decrease intracranial pressure (ICP). But could less really be more? Surgeons at Massachusetts General reviewed 229 patients with one of these monitors, looking at outcomes and complications. They found the following interesting results:
- There was no difference in mortality between the two monitor types
- The EVD patients did not require surgical decompression as often, possibly because of the ability to decrease ICP through drainage
- The EVD patients were monitored longer, and had a longer ICU length of stay. This was also associated with a longer hospital length of stay.
- Complications were much more common in the extraventricular drain group (31%). The most common complications were no drainage / thrombosis (15%) and malposition (10%). Hemorrhage only occurred in 1.6% of patients.
- Fiberoptic monitors had a lower complication rate (8%). The most common was malfunction leading to loss of monitoring (12%). Hemorrhage only occurred in 0.6% of patients.
Bottom line: Don’t change your monitoring technique yet. Much more work needs to be done to flesh out this small retrospective study. But it should prompt us to take a critical look for better indications and contraindications for each type of monitor.
Reference: Intraparenchymal versus extracranial ventricular drain intracranial pressure monitors in traumatic brain injury: less is more?J Am Coll Surg 214(6):950-957, 2012.