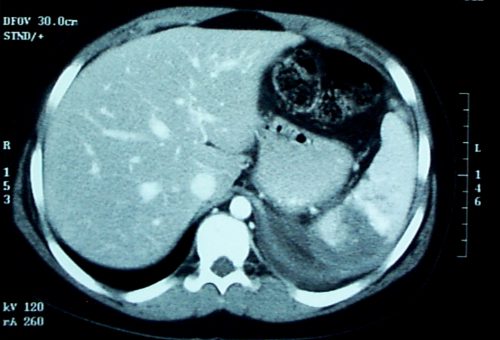
In the last two posts, I reviewed contrast anomalies in solid organs, specifically the spleen. Today, I’ll be more general and examine a recent paper that compared management and outcomes after the other major solid organ injury, liver, at Level I vs Level II trauma centers.
There are several papers that have detailed overall differences in outcomes, and specifically mortality, at Level I and II centers. Some of these show outcomes that are not quite as good at Level II centers when compared to Level I. On paper, it looks like these two levels should be very similar. Take away research and residents, and maybe a few of the more esoteric capabilities like reimplantation, and aren’t they about the same?
Well, not really. They can be, though. Level I criteria are fairly strict, and the variability between difference Level I centers is not very great. Level II criteria are a bit looser, and this allows more variability. Many Level II centers function very much like a Level I, but a few are only a bit higher functioning than a Level III with a few extra surgical specialists added in.
A paper currently in press used the Michigan Trauma Quality Improvement Program (MTQIP) data from all 29 ACS verified Level I and II centers in the state (wow!). Six years of information was collected, including the usual demographics, outcome data, and management. A total of 538 patients met inclusion criteria, and this was narrowed down to 454 so statistical comparisons of similar patients could be made for Level I vs Level II centers.
Here are the factoids:
- Mortality was significantly higher in Level II centers compared to Level I (15% vs 9%) and patients were more likely to die in the first two days, suggesting hemorrhage as the cause
- Patients were more likely to die in the ED at Level II centers, despite a significantly lower Injury Severity Score (ISS)
- Pneumonia and ARDS were significantly more likely to develop in Level II center patients
- Level II centers used angiography less often and took patients to the OR more frequently
- Level II centers admitted fewer patients to the ICU, but ICU admission was associated with significantly decreased mortality
- Complications were fewer at Level II centers, but they were less likely to rescue patients when they occurred
Bottom line: Level I and II centers are supposed to be roughly the same, at least on paper. But a number of studies have suggested that there are more disparities than we think. Although this paper is a retrospective review, the sheer number of significant differences and its focus on one particular injury makes it more compelling.
So what to do? Tighten up the ACS Orange Book criteria? That’s a slow and deliberate process that won’t help our patients now. The quickest and most effective solution is for all centers to adopt uniform practice guidelines so they all perform like the highly successful Level I programs in the study. There are plenty of them around. If you are not yet using one, I urge you to have a look at the example below. Tweak it to fit your center. And use your PI program to trend the outcomes!
Related post:
Reference: Variability in Management of Blunt Liver Trauma and Contribution of Level of ACS-COT Verification Status on Mortality. J Trauma, in press, Dec 1, 2017.