A reader sent a query yesterday regarding treatment of rib fractures, and specifically asking about epidural analgesia. Today, I’ll try to answer those questions.
Rib fractures, with or without other injuries, are a big killer in trauma patients. This is particularly true in the elderly. Overall mortality rates range from 3% to 13%, with the most import factor being pain. So what is the best way to manage patients with rib fractures to speed their safe recovery?
It’s best to attack this problem from three different directions simultaneously: pain control, respiratory hygiene (or pulmonary toilet if you’re a pessimist), and activity management.
There are many approaches to pain management, which include:
- Oral or IV analgesics
- Various types of blocks (intrapleural, intercostal, paravertebral, epidural)
- Topical agents (xylocaine patch)
- Stabilization (surgical only; belts and straps are bad for breathing)
Epidural analgesia is usually seen as the ultimate form of pain control, and is usually recommended for patients with multiple fractures or severe pain with inadequate response to medications and blocks. Much of the literature on its use is based on ICU patients who were not injured. A meta-analysis was conducted that specifically looked at epidural analgesia results in trauma patients, and found that it did improve pain management and some pulmonary function tests. However, there did not appear to be any change in mortality, ICU or hospital length of stay, or time on a ventilator.
Respiratory hygiene may involve simple measures such as coughing and deep breathing, incentive spirometry, and even mechanical ventilation in severe cases. Activity management consists of turning, sitting in a chair, walking, and forms of mechanical chest wall oscillation.
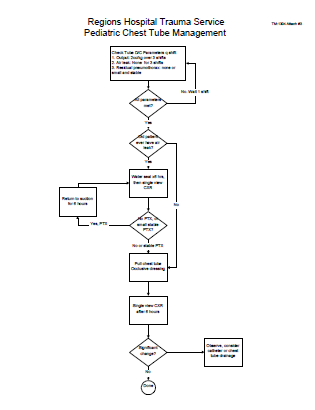
Bottom Line: The key to rib fracture management is a systematic approach that address all three dimensions of care based on objective patient measures. One size does not fit all, so more aggressive measures are warranted for more severe injury. I’ve attached an interesting patented scoring system and management algorithm, as well as two protocols from US trauma centers that range from simple (Vanderbilt) to more complex (West Virginia University).
Please feel free to comment, and I’d be happy to look at your protocol. Please email it to me!
Related post: History of epidural analgesia
Downloads
References
- Effect of epidural analgesia in patients with traumatic rib fractures: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth 56(3):230-42, Epub 2009 Feb 11.
- Rib Fracture Score and Protocol, US Patent #7,225,813 B2 – June 5, 2007