Trauma professionals worry about stuff. Like just about everything, really. Sometimes we have good guidance (research) to help us decide what to do. Many times, we don’t. Management of rhinorrhea and otorrhea from CSF leak after trauma is definitely one of those things.
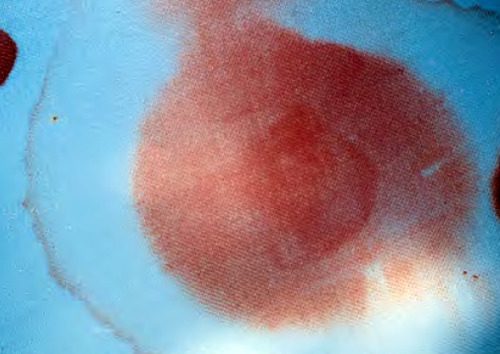
I’ve seen a variety of treatments used in these patients over the years. Is it really a CSF leak? Let’s get a beta-2 transferrin test (see below). Can’t the patient get meningitis? Their may be concomitant sinus fracture and bacterial contamination, so why not give antibiotics? Or vaccinate them?
The Cochrane library contains a vast number of reviews of common clinical questions. One of those questions just happens to be the utility of giving prophylactic antibiotics in patients with basilar skull fracture. Interestingly, they’ve been reviewing and re-reviewing this question about every 5 years, since 2006. During the three reviews done, there have been no additional research papers published on the topic.
Here are the factoids:
- Studies that specifically examined the use of prophylactic antibiotics in patients with basilar skull fracture were reviewed. All included meningitis as one of the outcome parameters.
- There were only 5 high quality (randomized, controlled) trials, with a total of 208 participants
- There were an additional 17 lower quality trials published, but no conclusions could be reached from them due to methodology problems
- In the high quality trials, there were no differences in the incidence of meningitis, mortality, or meningitis-related mortality
- There were no specific adverse effects related to antibiotic administration. But one of the high quality studies did note a shift to higher counts of pathologic bacteria in the posterior nasopharynx in the antibiotic group.
- No studies on the use of meningitis vaccinations exist. A survey of UK physicians showed that 35% recommend at least one vaccine, typically for Strep Pneumo.
Bottom line: There is still no good evidence to support the use of prophylactic antibiotics or meningitis vaccination in patients with CSF leak from uncomplicated basilar skull fracture. When you see surveys that show some physicians promoting a treatment and others doing nothing, it means there is most likely no significant benefit. If there were a big difference, we would have seen it by now! And giving drugs (antibiotics, vaccines) that have no proven use is expensive and can always lead to unexpected complications.
References:
- Immunisations and antibiotics in patients with anterior skull base cerebrospinal fluid leaks. J Laryngol Otol 128(7):626-629, 2014.
- Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst Rev April 28, 2015.