The trauma season is always officially open. And unfortunately, our patients can sustain mangled extremities in any number of ways. In days of old, management was simple: take it off. But we’ve become wiser over the years and are now able to salvage a good number of these threatened limbs. The Mangled Extremity Severity Score (MESS) has helped greatly with this. 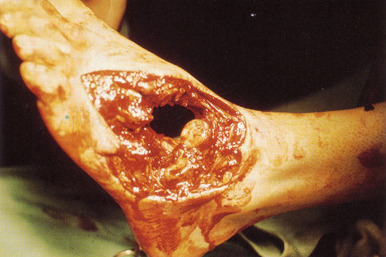
As I mentioned yesterday, it’s beginnings were humble, almost looking like guesswork on the part of the authors. But this system has withstood the test of time.
There are four components to MESS: limb ischemia, patient age, presence of shock, and mechanism of injury. Each component is assigned an integer value depending on severity. The possible values range from 1 to 14. Here’s the breakdown of each component:
Ischemia
- +1 Reduced pulse but normal perfusion
- +2 Pulseless, paresthetic, reduced capillary refill
- +3 Cool, paralyzed, insensate
- Add 3 points if limb ischemia has been present more than 6 hours
Age
- +0 <30 years
- +1 30-50 years
- +2 >50 years
Shock
- +0 SBP >90 consistently
- +1 Transient hypotension
- +2 Persistent hypotension
Mechanism (kinetic energy)
- +1 Low (stab, gunshot, simple fracture)
- +2 Medium (dislocation, open or multiple fractures)
- +3 High (high speed MVC, rifle)
- +4 Very high (high energy trauma with gross contamination)
Per the original study, values of 7 or greater predict low salvageability. However, with advancing technology, drugs, and operative techniques, the threshold has been creeping higher. But not that much higher, probably 8 or so.
Bottom line: Use the MESS score as one tool in your armamentarium to help address mangled extremities. But remember, it is not the final answer. In the OR, confer with your orthopedic and vascular colleagues. Decide if immediate amputation is necessary, or whether a second look in a day or two is in order. Use MESS as a tiebreaker. But remember, don’t let your desire to save the extremity jeopardize your patient’s life (rhabdomyolysis, renal failure, acidosis). If systemic signs begin to occur, cut your (and their) losses and amputate!
Related post:
