Yesterday, I presented a case of a young man with a knife in his back. He was brought to your ED in the prone position. The question was, what to do next?
With any trauma patient, regardless of size, shape, or position, the first question is always, “does this patient belong in the ED?” And usually, that question is answered by checking hemodynamic stability.
This patient stays prone while you quickly assess vital signs. If vitals are abnormal, he needs to get rolled to the operating room immediately, while still prone. There is no time to figure out how to reposition, or if the knife can be removed. Get him out of your ED.
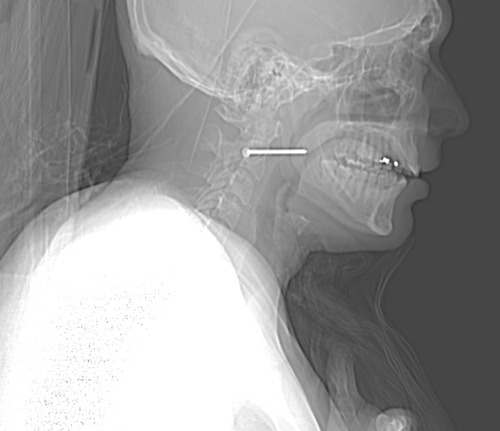
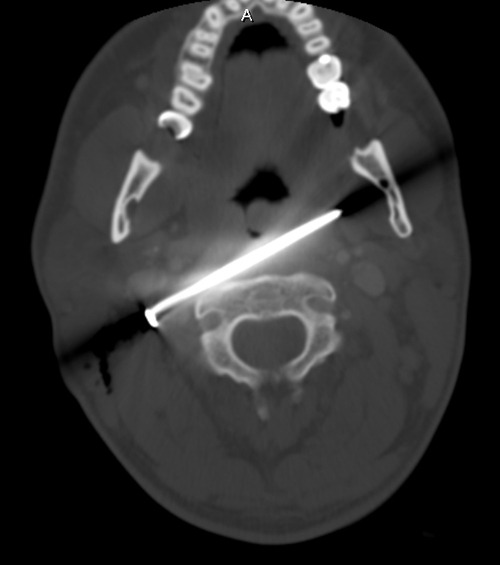
But let’s say he is hemodynamically normal and talking to you. You need more information. So start with a physical exam. With him in the prone position! It works. In this case, there are no other puncture wounds, and the anterior part of the body can be examined by carefully logrolling him onto his side. Breath sounds are decreased over the right chest, otherwise there are no other anomalies.
So now what? Well, let’s get some more info! How about a chest xray? Best position? Prone! It’s the easiest, because the patient does not need to be held up next to an xray plate, which would also have to be held manually. The lateral view doesn’t add anything but hassle. Here’s the result:
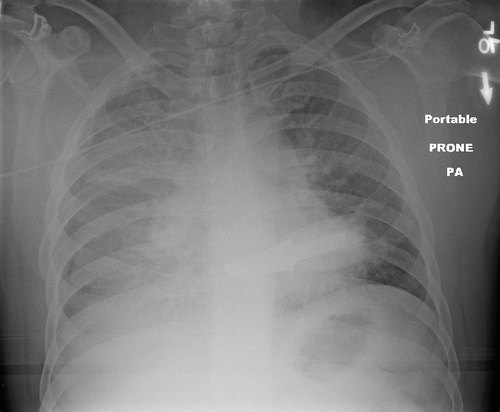
Now what? What do you see, what do you do? Tweet or comment; more to follow tomorrow.
Related post: