Angioembolization has become a common procedure that can increase the likelihood of success for nonoperative management for splenic trauma. It does have its own set of complications to be aware of, however.
The most obvious complication is mechanical injury to the femoral artery. This occurs in 1 to 3% of patients. It is more common in the very young (small caliber artery) and the elderly (arteries of stone). Rarely, the substance or device that is used for the embolization may migrate or end up on the wrong spot, infarcting something important.
A common issue that occurs is infarction of portions of the spleen. This is actually the desired effect, as it stops the bleeding. Most of the time, we are unaware of the changes that take place in the spleen post-procedure. But every once in a while we get a repeat CT scan days or weeks down the road and see some very interesting things.
The most common finding is a splenic infarct alone. This is an area of the spleen, sometimes wedge shaped, that does not take up contrast. This is normal. In some cases, gas bubbles are seen within the spleen parenchyma, usually within the infarcted area. In others, large areas of gas are present, and an air-fluid level may also be seen. This is definitely not normal.
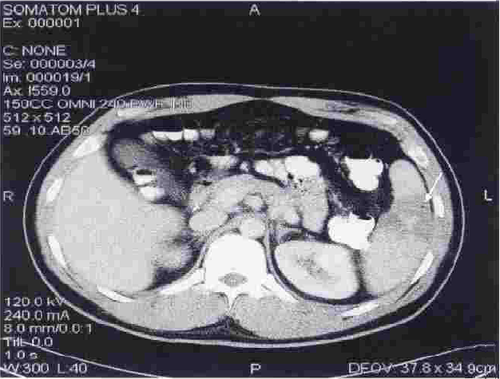
Note the infarcted area at the arrow, with a tiny gas bubble visible.
Tiny bubbles are normal after this procedure, and can be ignored if the patient does not appear ill and does not have any systemic evidence of inflammation or sepsis. On the other hand, big bubbles or air-fluid levels probably indicate a developing splenic abscess, and the patient will usually appear ill and have a high WBC count. Unfortunately, the only treatment for this is splenectomy. Insertion of drainage catheters does not work and the patient will only become sicker if it is attempted.
