Deep venous thrombosis (DVT) and pulmonary embolism (PE), collectively known as venous thromboembolism (VTE), are major concerns in all hospitalized patients. A whole infrastructure has been developed to stratify risk, monitor for the presence of, and provide prophylactic and/or therapeutic drugs for treatment. But if you critically look at the literature from the past 20 years or so, we have not made much progress.
One of the newer additions to our arsenal has been to figure a way to determine the “optimal” dose of enoxaparin. Three options are now available: weight-based dosing, confirmation by thormboelastography (TEG), and anti-factor Xa assay. Let’s look at another paper that focuses on the last item.
Anti-factor Xa levels provide a way to monitor low molecular weight heparin activity. A number of papers published have sought to determine a level that predicts adequate activity. Although they are not of the greatest size or quality, a range of 0.2-0.4 IU/ml seems to be the consensus.
A large number of patients at a busy Level I trauma center were retrospectively studied to see if achieving a peak anti-factor Xa level of at least 0.2 IU/ml would result in less VTE. All patients were started on enoxaparin 30mg SQ bid within 48 hours of admission. Anti-factor Xa was measured 4 hours after the third dose. If the level was less than 0.2 IU/ml, the dose was increased by 10mg per dose. The cycle was repeated until anti-factor Xa was therapeutic.
Here are the factoids:
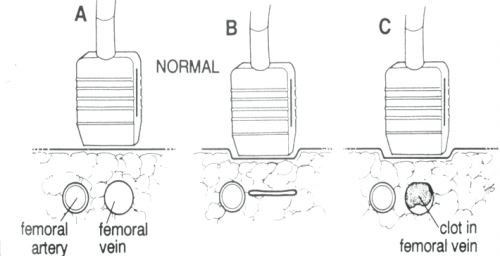
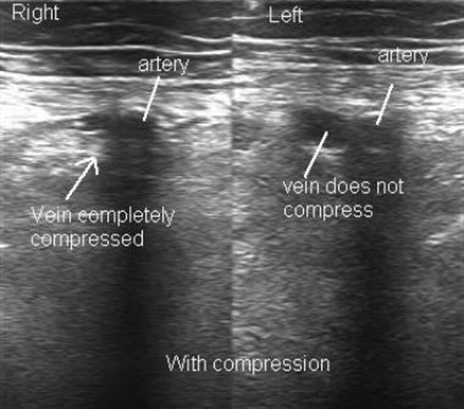
- All patients with a Greenfield Risk Assessment Profile (RAP) of 10 or more (high risk) were included; duplex ultrasound surveillance for lower extremity DVT was performed weekly
- 194 patients were included, with an average RAP of 9 and ISS of 23 (hurt!)
- Overall VTE rate was 7.4%, with 10 DVT and 5 PE (!)
- Median time to diagnosis was 14 days
- Initial anti-factor Xa levels were therapeutic in only one third of patients, and another 20% reached it after dose increases. 47% never achieved the desired level, even on 60mg bid dosing.
- There was no difference in DVT, PE, or VTE rates in patients who did vs did not achieve the goal anti-factor Xa level
- Injury severity and obesity correlated with inability to reach the desired anti-factor Xa level
Bottom line: In this study, achieving or not achieving the goal anti-factor Xa level made no difference whether the patient developed VTE or not. And it was difficult to achieve anyway; only about half ever made it to the desired level. How can this happen?
Well, there are still many things we don’t understand about the genesis of VTE. There are probably genetic factors in every patient that modify their propensity to develop it after trauma. And there are certainly additional mechanisms at play which we do not yet understand.
For now, we will continue to struggle, adhering to our existing protocols until we can figure out the real reason(s) VTE happens, the best ways to prevent, and the best methods to treat.
Related posts:
- Anti-Xa levels: who cares -Part 1
- Anti-Xa levels: who cares – Part 1.5
- Anti-Xa levels: who cares – Part 2
- Anti-Xa levels: who cares – Part 3
Reference: Relation of Antifactor-Xa peak levels and venous thromboembolism after trauma. J Trauma accepted for publication Aug 2, 2017.