You’re doing one of those (very rare) DPLs and get a surprise result. Not blood, not obvious intestinal content, but just a small amount of mysterious sediment. What to do?
Well, this is obviously not normal. Therefore, this has to be considered a positive diagnostic peritoneal lavage. Since DPL is a qualitative test (meaning that the answer is only yes or no), the patient must go to the OR.
Here are the answers to the questions posed earlier today:
- The DPL catheter has a relatively small diameter, so leave it in place! It may be very difficult to find where it went otherwise
- Midline laparotomy incision is most appropriate. Remember, this is a trauma case? However, you can start infra-umbilical with a limited incision.
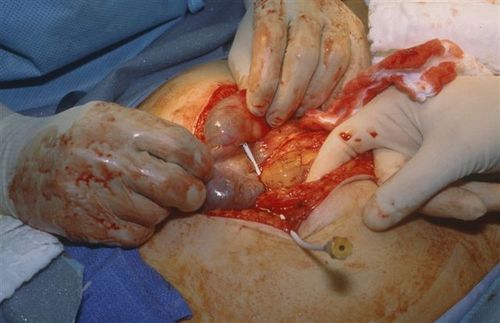
Here’s what I found in this case:
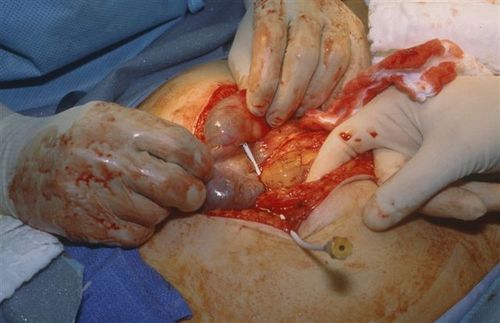
The catheter went straight into the cecum! So we actually did a diagnostic colonic lavage! The sediment was a very small amount of stool. And as stated above, had the catheter not been left in place, it would have been very tough to find the puncture site.
Next, I clamped the catheter to keep it in place, cut it on the hub side, and removed most of it.

Finally, I placed a purse-string stitch around the entry site in the bowel, removed the catheter and tied the suture.

But wait, we’re not done yet! The patient did have abdominal pain and a seat belt sign, so we did a trauma exploration through the midline incision. A Grade II liver injury was present which needed no further management. The patient did well and was discharged on the fourth day.
Bottom line: Procedures can and do go awry. Reason your way through it the best you can, then use focused diagnostics, if needed, to come up with a plan. For misplaced needles and catheters, most organs can tolerate a puncture by almost anything (except the eye, maybe). Treat appropriately and monitor carefully afterwards.
Source: Personal archive. Not treated at Regions Hospital