Recommendations for open fracture management has evolved over the past 20 years. The old-timey rule used to be: all open fractures need to be treated within 8 hours. This treatment could be washout and ORIF, washout and external fixation, or just washout alone. The washout was the constant across all types of management.
Then the orthopedics literature began to suggest that “lesser” fractures (Gustilo I – II) could go a bit longer. Some centers extended their required time to washout up to 12 or even 16 hours. Subsequently, the value of early IV antibiotics was recognized, and the time to washout started to change again.
Now, we have recommendations for early IV antibiotics competing with the old recommendations for prompt washout. Who is winning?
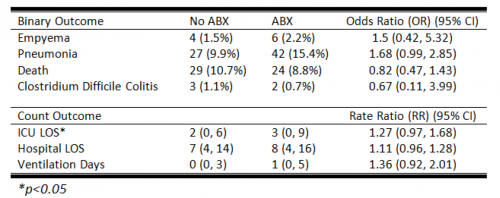
There are two recent papers that seem to provide conflicting recommendations regarding antibiotics. The first is in process for publication by the ortho group at San Francisco General Hospital. They studied 230 open fracture patients at their Level I Trauma center over a five-year period. They monitored for surgical site infection that occurred during the first 90 days after injury.
Here are the factoids:
- It took 450 consecutive patients to find the 230 study patients due to these exclusion criteria: missing documentation of antibiotic administration, delayed presentation, and loss to followup
- There were 169 Gustilo Type I or II fractures and 61 Type III fractures
- They noted a trend (p = 0.053) toward infection in patients who had antibiotic administration an average of 83 minutes after arrival vs those who received them within one hour
- Patients who received their antibiotics 2 hours after arrival had a 2.4x increase in likelihood for infection within 90 days
But there was another paper published in the same journal this year that shows the opposite result. This one is from the University of Bristol in the UK. This one reviewed only Gustilo Type III fractures and observed changes in the deep infection rate, before and after the National Health Service guidance on antibiotic administration changed from within three hours to one hour post-injury.
Some more factoids for you:
- A total of 176 patients were identified at a single center, and only 152 were left after the usual exclusions
- Average time to antibiotic administration decreased from 180 minutes to 160 minutes after the new guidance was issued (60 minutes(!))
- Only 12 patients developed deep infections with a median followup of 26 months
- On regression analysis, no obvious factors for increased risk were identified
Bottom line: So what gives? Two different answers: antibiotics given after 2 hours is associated with an increased risk of infection, vs no difference?
No, not really. Talk about apples to bananas. The first study looks at all open fractures, not just the most severe. It does not really define “surgical site infection,” so can we assume it was any infection? We don’t know. The second study looked only at deep infections.
The sample sizes are marginal in both studies, although the first was able to show a significant result despite this. And, of course, these are association studies, so other factors could be at play to manifest an infection or not. Both groups showed an 8-11% infection rate of some kind in their Gustilo Grade III fractures.
But the biggest issue with the second study is that, despite guidance that antibiotics should be given within an hour, the average time decreased from 3 hours to only 2:40. This is still beyond the two hour threshold to higher infection rates suggested in the first paper.
So what do I make of all of this? The UK paper is lacking the power and enough of a treatment change to be taken seriously. The San Francisco paper shows borderline results with a 2.4x increase in all infections if antibiotics are given after 2 hours.
So until we have better data and larger series, 1 hour antibiotic administration seems like a painless way to decrease the likelihood of an infection. But whether that can safely delay the time to washout remains to be seen.
References:
- Delay of Antibiotic Administration Greater than 2 Hours Predicts Surgical Site Infection in Open Fractures. Injury, in press, May 29, 2020.
- Time to intravenous antibiotic administration (TIbiA) in severe open tibial fractures: Impact of change to national guidance. Injury 51:1086-1090, 2020.