Portable CT Scanning For Trauma Patients
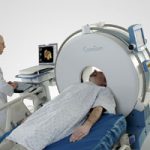
I recently had the opportunity to see a portable head CT scanner in action, the CeroTom by NeuroLogica (Danvers, MA). Today, I’ll give my thoughts on this new technology.
There are 3 major considerations when evaluating portable CT scanning:
- Patient safety, always at the forefront
- Usefulness, also know as image quality
- Financial viability
From a safety standpoint, portable scanning can decrease (but not eliminate) the safety hazards associated with transporting a critically ill patient out of the ICU. Road trips are associated with misplaced/displaced lines, tubes and monitors about 15% of the time. These are lifelines in some patients, and even momentary disruptions can be life-threatening. Some patients are on levels of support so high they are not transportable, so portable scanners offer an opportunity to get diagnostic imaging that would not be available otherwise.
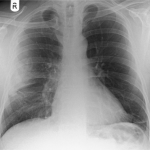
Clinical performance is on par with standard scanners. Resolution is lower, but the diagnostic accuracy and reliability are not different compared to fixed scanners.
From a financial standpoint, use of the portable scanner works as well. The Cleveland Clinic deployed a CereTom scanner a few years ago and found that the unit paid for itself in 6.9 months. For you financial types, the internal rate of return was 169% and the 5-year expected economic benefit was $2.6 million.
Bottom line: This new piece of technology offers significant benefits to patients in the ICU who may otherwise not be able to get imaging due to safety reasons. It can also be employed in the OR on anesthetized patients, which can assist with diagnosis in patients with both abdominal injuries requiring immediate operation and concomitant head injury.
Practical notes: The CereTom is an 8-slice scanner with a 25cm field of view. The patient is moved onto a scan board which supports the head while it is moved slightly off the top of the bed to accommodate the scanner. Current scanner cost is $450,000 and attachment packages for hospital beds are $7,000. One CT technologist can operate the unit, which takes about 5 minutes to set up and 15 minutes to scan. All lines, tubes and monitors must be (carefully) moved to the side of the bed so the scanner can fit over the top.
References:
- The economic and clinical benefits of portable head/neck CT imaging in the intensive care unit. Radiology Manage 30(2):50-54, 2008.
- Review of portable CT with assessment of a dedicated head CT scanner. Am J Neuroradiol 30:1630-1636, 2009.
I have no financial interest in Neurologica, Inc.