Yesterday, I described a case of a young athlete who developed progressive back pain after rapidly increased his deadlift weights. He presented to the hospital with back pain and inability to get up from a supine position. He had firm and tender paraspinal muscles in his lower back, but no other findings.
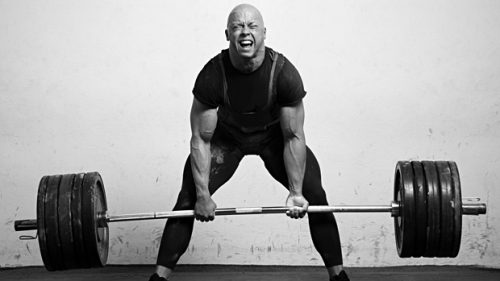
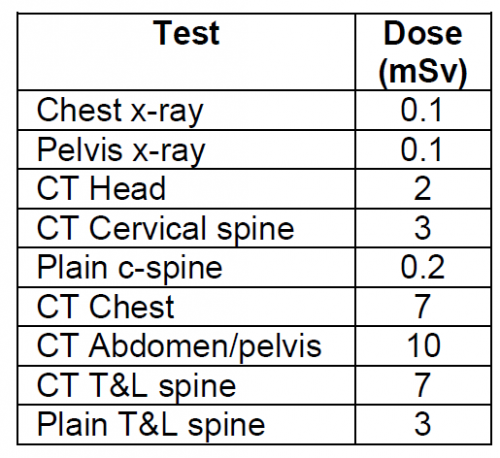
What to do next? Obviously, we need a bit more information on the bony structures. Other than run of the mill muscle strain, a compression fracture would be the next most common diagnosis. In this young, healthy athlete, a simple set of AP and lateral spine images should be sufficient. But if you opted for a CT scan, I won’t argue. In either case, the images were normal.
Since there is significant muscle pain and tenderness, a lab panel with a few extras is in order, as well. The usual electrolytes, etc were normal. Creatinine was 0.9, but CPK was 60,000!
Now what are you thinking? What’s the diagnosis, and what is the decision tree for treatment?
Add your comments below, or tweet them out. I’ll finish this topic up in the next post.