I’ve previously blogged about the flat vena cava sign as an indicator of low volume status in trauma patients. One of the papers at EAST takes another look at this tool, and had a surprisingly negative result.
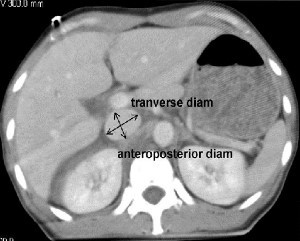
A retrospective study at George Washington University was carried out over a one year period. They looked at all of their highest level trauma activation patients who also underwent CT scan of the abdomen. Images were read by three radiologists and inter-rater reliability was reviewed. The transverse to anteroposterior diameter ratios were calculated to determine flatness.
Here are the factoids:
- 276 patients met enrollment criteria, and were mostly male and blunt trauma
- The IVC was nearly round in 21% of patients and collapsed in 26%
- There was no association between IVC shape and shock index, blood pressure, Hbg, lactate, urgent operation, angiography or length of stay
- There was also no association between IVC shape and blood transfusion or death
- Correlation of the reads between radiologists was good
So what gives? A paper I reviewed three years ago in the Journal of Trauma came to a different conclusion. They found that a flat IVC on CT scan (defined as a transverse to AP ratio of 4:1 or greater) was associated with a significantly higher chance of receiving more crystalloid or blood, as well as requiring an operation within 24 hours.
First, the newer work is an abstract, so a lot may be unsaid at this time. This is why I encourage everyone to always read the entire paper! The published paper involved a smaller series (114 patients), but it was prospective and had reasonable statistical analyses.
Bottom line: This is a presentation that I’ll have to sit through and ask the authors why they didn’t find the same results as the older paper. For now, continue to use the flat IVC sign as a potential sign of trouble ahead. I’ll report more on this one later in January.
Reference:
- Inferior vena cava size is not associated with shock following injury. EAST 2014, oral paper 12.
Related post:


