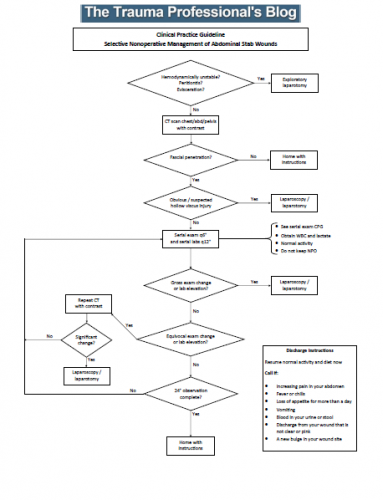
Gunshots to the abdomen are a no-brainer that nearly always require operative exploration, but stab wounds are more challenging. They are low velocity, and injury only occurs in the pathway of the knife. It is more likely that inconsequential (or no) injuries occurred. Since exploratory laparotomy (or even laparoscopy) is not a benign procedure, trauma professionals frequently opt for selective nonoperative management (observation) in these cases.
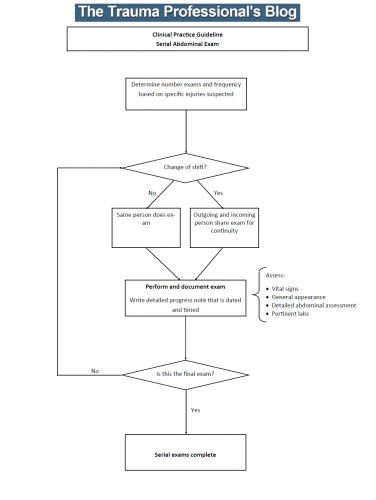
What does observation mean? The patients are kept in the hospital for a set period of time, receive serial abdominal examinations, and get a few repeat lab tests. If the exam changes, the patient is taken to the OR to find out why. If it doesn’t, they are fed and sent home.
But what is the appropriate period of time to observe? One major concern is for the possible hollow viscus injury. Stomach and colon contain fluids that cause prompt peritonitis. But small intestinal content is rather innocuous, with neutral pH, normal concentration, and few bacteria. Peritonitis may not occur for days. Yet most centers send these patients home within 12 to 24 hours of injury.
What is the right answer? The trauma group at LAC+USC in Los Angeles performed a prospective, observational study to try to answer the question. They enrolled all patients with abdominal stab wounds presenting to their center over a three year period. They were generous (and correct) with their definition of the abdomen, including the thoracoabdominal portion up to the 5th intercostal spaces, and the pelvis.
Patients were excluded if they were hemodynamically unstable, or had an evisceration or obvious peritonitis. Most patients received a CT scan, and patients with suspected hollow viscus injury were excluded from the study and taken to the OR. All others were observed in a dedicated unit and were monitored for change in exam, need for blood transfusion, or other event which was recorded for the study.
Here are the factoids:
- A total of 256 patients met study criteria: 77% had a single stab and 76% had a negative FAST exam
- There were 46 patients who underwent immediate laparotomy for evisceration (59%), hemodynamic instability (33%), or peritonitis (24%)
- 81% of patients underwent CT scan, and 13% were taken to OR based on the findings
- This left 210 patients for nonoperative management
- Of these, 71 had positive scans and all were due to solid organ injury. One patient failed at 32 hours due to increasing lactate and WBC, but the operation was nontherapeutic.
- Another 14 patients had equivocal CT findings and two failed at 10 and 20 hours due to small bowel injury discovered by increasing lactate, WBC, change in exam, and air on a repeat CT
- All 123 patients with negative scans passed nonoperative management
- Median hospital length of stay was 3 with a range of 2-6 days
Since all of their patients who failed observation did so within 24 hours, the authors recommended a 24 hour observation period for all patients with stabs to the abdomen who did not meet their exclusion criteria.
Bottom line: Trauma professionals have needed a study like this for decades. Until now, we’ve been flying by the seat of our pants, with each surgeon making up his or her own magic number. This is a well done first attempt at defining what that number should be.
Yes, there are some limitations to the study. The most important one that we don’t know the answer to is how many patients were successfully discharged that presented to another hospital with complications or failure. But this study provides a very reasonable estimate that helps us balance the cost (and patient inconvenience) of time in the hospital vs the dangers of a delayed diagnosis.
The only thing that remains is to design the practice guideline that incorporates the observation period, how often serial exams and labs should be obtained, and when the CT should be repeated.
Reference: Prospective evaluation of the selective nonoperative management of abdominal stab wounds: When is it safe to discharge? Journal of Trauma and Acute Care Surgery: November 2022 – Volume 93 – Issue 5 – p 639-643.