Helicopter EMS (HEMS) transports are a valuable yet very expensive resource. Unfortunately, many state trauma systems or local EMS agencies do not provide specific guidance for best use. A group at the University of Alabama in Birmingham performed a geospatial analysis of helicopter transports in their area to determine the efficiency of HEMS operations.
This group created a sort of “heat map” that showed the number of transports overlaid on a geographical map of their catchment area. It included HEMS transports over a 6-year period directly from the scene. Drive and flight times were calculated, and the latter also included flight time to reach the scene.
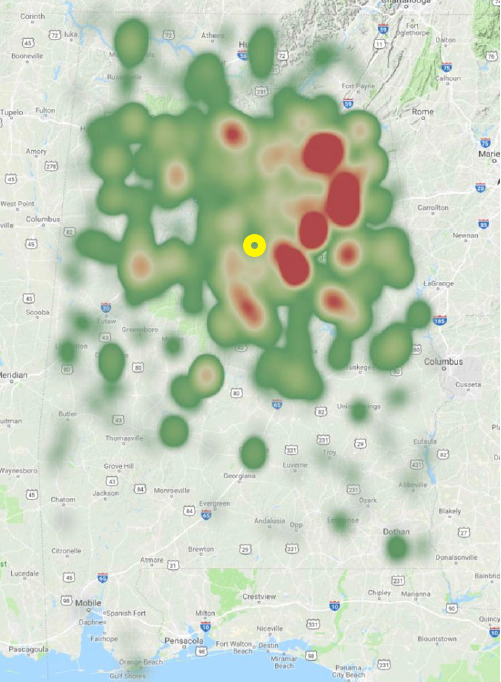
Here’s the heat map showing the entire state of Alabama. The approximate location of Birmingham is indicated in yellow.
Here are the factoids:
- Nearly 3000 patients were identified, and 1911 had scene locations recorded so analysis could be performed
- 35% of patients had minor injuries with ISS 1-8 (!!)
- Median flight time was 58 minutes, and median drive time was only 65 minutes
- In 28% of cases, drive time would have been shorter than flight time when considering time for the helicopter to reach the scene
- Conclusion: over one fourth of patients might have arrived at the hospital more quickly by ground ambulance
Here are some questions for the authors and presenter to consider in advance to help them prepare for audience questions:
- Why include time for the helicopter to reach the scene but not a ground ambulance? Doesn’t this stack the deck in favor of ground transport?
- Was there any correlation between scene proximity and high ISS? This might have been a reason for calling the helicopter.
- Did you see any patterns in the low ISS group? This could provide insight into the EMS thought processes. These patients are potentially the low hanging fruit to direct educational activities to reduce HEMS use.
This is thought-provoking work and I look forward to hearing all the details!
Reference: Use of helicopters for retrieval of trauma patients: a geospatial analysis. EAST 2019, Quick Shot Paper #26.