Over the past two days, I’ve reviewed the new AAST organ injury scaling updates for spleen and liver injuries. Today, I’ll cover the new kidney grading scale.
Liver and spleen grading is generally simple, focusing on laceration depth and subcapsular hematoma coverage to determine the exact value. However, the kidney is totally different. Although technically a solid organ, it’s got a bunch of hollow, urine-containing stuff inside. This is the main determinant of the original scaling system: collection system involvement.
Like liver and spleen, the kidney scale was updated to take advantage of CT information. But once again, bleeding identified via the CT angiogram is incorporated into the higher grades. Active bleeding contained within Gerota’s fascia is assigned a grade of III. Extravasation escaping this fascia is assigned a IV. The other grades remain unchanged.
Here are the updated guidelines. Click the image or link below it to open a bigger image in a new window.
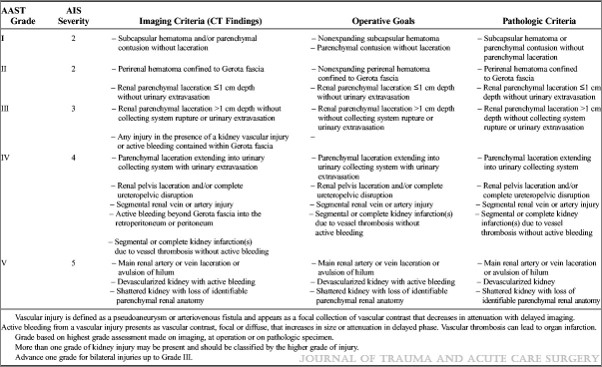 Click to download larger image
Click to download larger image
Links:
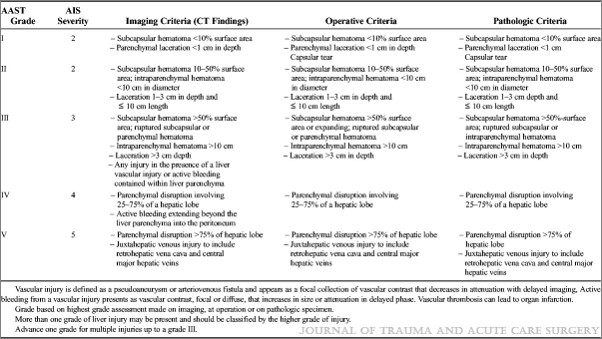
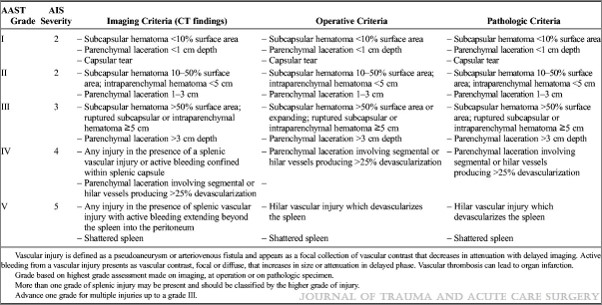
- Updated AAST spleen scaling system
- Updated AAST liver scaling system
- Updated AAST kidney scaling system