Many trauma centers have moved toward reversing warfarin with prothrombin complex concentrate (PCC) in place of plasma due to the speed and low volume of infusate with the former. In the US, 3-factor PCC was approved by the FDA first, but it has a lower Factor VII content. This usually required infusion of plasma anyway to make up the Factor VII, so what was the point (although there was some debate on this)?
Then 4-factor PCC was approved, and it alone could be used for warfarin reversal. But so far, PCC has not been routinely used for reversal of coagulopathy from trauma. We still rely on plasma infusion for this. The abstract I am discussing today compares reversal with 4-factor PCC alone to reversal with 4-factor PCC and plasma in coagulopathic patients.
This study retrospectively reviewed adult patients who received one of the above treatments over a 3 year period. Patient who were on oral anticoagulants were excluded. The goal INR was 1.5, and time to correction and number of PRBC transfused were measured.
Here are the factoids:
- There were 516 patients who met criteria, but only 80 FFP patients and 40 PCC+FFP patients were analyzed
- Patients were an average of 58 years old, had an ISS of 29, and 87% had sustained blunt injury
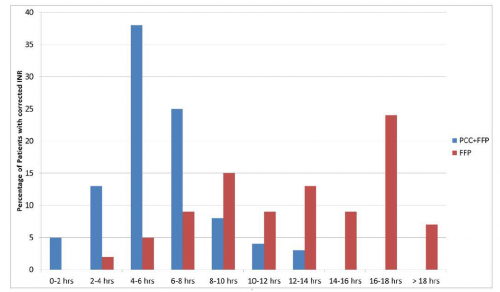
- PCC+FFP resulted in faster correction of INR (373 min vs 955 min)
- PCC+FFP received fewer units of PRBC (7 vs 9 units) and FFP (5 vs 7 units)
- Mortality rate was lower in the PCC+FFP group (25% vs 33%)
- There was no difference in thrombotic complications
Bottom line: Well, this is an interesting start. I think this abstract suggests that we should incorporate giving 4-factor PCC into the massive transfusion protocol to try to reduce the INR faster. However, the patient numbers are low and several of the results are only weakly significant (units transfused, mortality, p=0.04). Some additional confirmative studies will be needed before this is ready for prime time!
Here are some questions for the authors to consider before their presentation:
- Why did your study group drop from 516 to 120? What impact might this have had on you analyses?
- Did you look at the correction times stratified by initial INR? Severely coagulopathic patients could skew the numbers, especially if they were predominantly in only one of the study groups.
- It did not look like the patients received much PRBC or plasma (<10 units of each). How injured / coagulopathic were they?
- The mortality rates are rather high for an average ISS of 29. Did you analyze to see what impact ISS had on mortality? Could this have influenced your analysis?
- Big picture question: Should we consider routinely giving PCC as part of the massive transfusion protocol in patients who are known to be coagulopathic? Based on the graph, it looks like patients will need more than a single dose. Reversal time was still very long for PCC+FFP.
Thanks for an intriguing abstract!
Reference: EAST 2018 Podium paper #12.

