There is tremendous variability in ordering imaging in trauma patients. To some degree, this is due to the dearth of standards pertaining to radiographic imaging, at least in trauma. And when standards do exist, trauma professionals are not very good at adhering to them. We’d rather do it our way. Or the way we were trained to do it.
The group at Jamaica Hospital in Queens, NY quantified some of those differences, studying ordering patterns of trauma surgeons (TS), emergency physicians (EP), and surgery chief residents (CR). Unfortunately, they then tried to draw some interesting conclusions, which I’ll discuss at the end.
They reviewed all blunt trauma activations over a 6 month period at their urban trauma center. At the end of each trauma activation, each of the three physician groups wrote imaging orders, but only the trauma surgeons’ were submitted. Missed injuries were defined as any that would not have been found based on each provider group’s orders. Extremity injuries, and those found on physical exam or plain imaging were excluded.
Here are the factoids:
- The authors do not state how many patients they saw in this period, but by extrapolation it appears to be about 250
- Trauma surgeons ordered significantly more studies (1,012) than the EPs (882) or CRs (884)
- This resulted in essentially a “pan-scan” in 78%, 64%, and 69%, respectively
- Radiation exposure was said to be the same for all groups (18 vs 13 vs 15 mSv) [I’m having a hard time buying this]
- But cost was higher in the trauma surgeon group ($344 vs $267 vs $292) [Huh? Is this only the electric bill for the CT scanner? Very low, IMHO]
- And the trauma surgeons had a missed injury rate of only 1%, vs 11% for EPs and 7% for CRs [Wow!]
Bottom line: Sorry, I just can’t believe these results. There are a lot of things left unsaid in this poster. What were all these missed injuries? What magical CT scan that only the trauma surgeons ordered actually picked them up? And probably most importantly, were they clinically significant? A small hematoma somewhere doesn’t make a difference (see the “tree falls in a forest” post below).
It looks to me like the authors wanted to justify their use of pan-scan, and push their emergency physicians to follow suit. Unfortunately, this is a poster presentation, meaning that there will be limited opportunity to question the authors about the specifics.
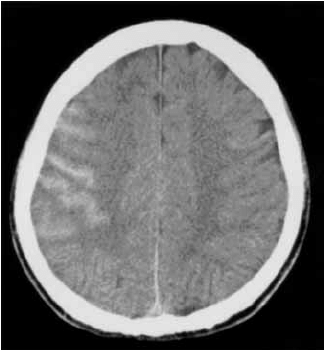
The debate regarding pan-scan vs selective imaging is an active one. The evidence is definitely not in yet. While we sort it out, the best path is to develop a reasonable imaging practice guideline based on the literature, where available. Some areas such as head and cervical spine CT have been worked out fairly well. Then fill in the blanks and encourage all trauma professionals in your hospital to follow them. There is great value in adhering to good guidelines, even when there are blanks in our knowledge.
Related posts:
- Sample Blunt trauma radiographic imaging protocol
- If a tree falls in a forest…
- Why create practice guidelines
Reference: Variability in computed tomography imaging of trauma patients among emergency department physicians and trauma surgeons with respect to missed injuries, radiation exposure and cost. AAST 2016, Poster #75.