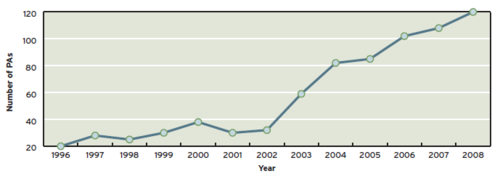
The number of physician assistants (PAs) and nurse practioners (NPs) moving out of primary care to work in specialty areas in US healthcare is rising. Trauma programs in teaching hospitals have been affected by the work hour restrictions put into place 10 years ago. Non-teaching programs have been adding these midlevel providers to help balance workloads.
How common is the use of midlevel providers in trauma care? Nine-item surveys were sent to 464 designated or ACS verified trauma centers across the US.
Here are the factoids:
- The response rate was 53%, which is very good
- It’s too bad that Level III and IV centers were excluded. There would have been some good data there.
- About half were ACS verified trauma centers. Also, roughly half were Level I and half were Level II.
- 35% used PAs, 33% used NPs, and 54% used residents. There was overlap in use.
- ACS verified centers used midlevels more frequently than non-ACS centers (62% vs 41%)
- Level I centers used them more than Level IIs (73% vs 53%)
- Trauma centers with residents used midlevels more often than those without (66% vs 41%)
- Midlevels were utilized for the traditional tasks of a surgical provider (H&P, discharge summary, rounds, trauma resuscitation, surgical assistant)
- A third performed procedures like chest tubes, arterial and central lines
- 19% of hospitals that did not use midlevels planned to start soon
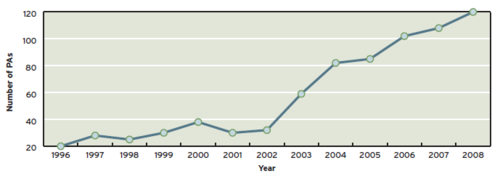
Bottom line: Midlevel providers such as PAs and NPs are being used more and more frequently in trauma care. If you look at the graph, the inflection point happened just around the time of the new work hour rules. We use them at our trauma center, and they are very prevalent at the centers I have visited. These providers are valuable clinicians and their contributions to patient care should be embraced!
As a side note (opinion), the amount of trauma slowly grows with the population. And the number of “trauma hours” spent to take care of these patients is a zero sum game. This means that resident exposure to trauma must be decreasing as midlevel provider involvement increases. Physician training in trauma (and all other disciplines as well) is shrinking, but at least they’re not tired!
Related post:
Reference: Acceptance of physician assistants and nurse practitioners in trauma centers. JAAPA 23(1):35-41, 2010.